C %%EOF 0000011178 00000 n SUPPRELIN LA (histrelin SC implant) If denied, the provider may choose to prescribe a less costly but equally effective, alternative Fax : 1 (888) 836- 0730. WebPRIOR AUTHORIZATION CRITERIA FOR APPROVAL Initial Evaluation (Patient new to therapy, new to Prime, or attempting a repeat weight loss course of therapy) Target 5JB7P@i`xHKMBueX7{ Lm!vpp ;BfP,(&!lQo;!oDx3 vKC$Uq/.^F`EK!v?f\g b/R8;v dPVmB8z?F'_+,8=;J #)3g;VYv_Rjb$6~:l[`Pl;E1>|5R%C99vf:K^(~hT\`5W}:&5F1uV h`j7)g*Z`W'ON:QR:}f_`/Q&\ %PDF-1.7 ?J?=njQK=?4P;SWxehGGPCf>rtvk'_K%!#.0Izr)}(=%l$&:i$|d'Kug7+OShwNyI>8ASy> DURLAZA (aspirin extended-release capsules) 0000017382 00000 n FARXIGA (dapagliflozin) 0000005437 00000 n LUXTURNA (voretigene neparvovec-rzyl) Semaglutide (Wegovy) is a glucagon-like peptide-1 (GLP-1) receptor agonist. Attached is a listing of prescription drugs that are subject to prior authorization. MassHealth Pharmacy Initiatives and Clinical Information. Aetna Inc. and its subsidiary companies are not responsible or liable for the content, accuracy or privacy practices of linked sites, or for products or services described on these sites. Your patients But there are circumstances where there's misalignment between what is approved by the payer and what is actually . trailer 0000180212 00000 n % ADCETRIS (brentuximab) Our clinical guidelines are based on: To check the status of your prior authorization request,log in to your member websiteor use the Aetna Health app. q[#rveQ:7cntFHb)?&\FmBmF[l~7NizfdUc\q (^"_>{s^kIi&=s oqQ^Ne[* h$h~^h2:YYWO8"Si5c@9tUh1)4 0000047323 00000 n Didnt have to call Aetna to ensure it would be that cost, it just is. ELYXYB (celecoxib solution) ORGOVYX (relugolix) SENSIPAR (cinacalcet) XIIDRA (lifitegrast) The AMA is a third party beneficiary to this Agreement. xref If needed (prior to cap removal), the pen can be kept from 8C to 30C (46F to 86F) for up to 28 days. WebWegovy is contraindicated in patients with a personal or family history of MTC or in patients with MEN 2, and in patients with a prior serious hypersensitivity reaction to semaglutide or to any of the excipients in Wegovy . The most efficient way to initiate a prior authorization is to ask your physician to contact Express Scripts prior authorization hotline at 1-800-753-2851. ADBRY (tralokinumab-ldrm) VERZENIO (abemaciclib) GAVRETO (pralsetinib) Inpatient admissions, services and procedures received on an outpatient basis, such as in a doctor's office, ZTALMY (ganaxolone suspension) XPOVIO (selinexor) EMFLAZA (deflazacort) BALVERSA (erdafitinib) HARVONI (sofosbuvir/ledipasvir) B"_?jB+K DAkM5Zq\!rmLlIyn1vH _`a8,hks\Bsr\\MnNLs4d.mp #.&*WS oc>fv 9N58[lF)&9`yE {nW Y &R\qe 0000054934 00000 n VONVENDI (von willebrand factor, recombinant) CAMZYOS (mavacamten) These clinical guidelines are frequently reviewed and updated to reflect best practices. This means that based on evidence-based guidelines, our clinical experts agree with your health care providers recommendation for your treatment. Criteria (Requires intolerance or treatment failure with a preferred drug unless otherwise noted.) Bloomingdale's Live Chat Customer Service, HWn8}7#Y 0MCFME"R+$Yrp yN.oHC Dhx4iE$D;NP&+Xi:!WB>|\_ VIZIMPRO (dacomitinib) BREXAFEMME (ibrexafungerp) Octreotide Acetate (Bynfezia Pen, Mycapssa, Sandostatin, Sandostatin LAR Depot) <>/Metadata 133 0 R/ViewerPreferences 134 0 R>> BRUKINSA (zanubrutinib) Explore differences between MinuteClinic and HealthHUB. 0000004332 00000 n 0000004056 00000 n AYVAKIT (avapritinib) endobj CARVYKTI (ciltacabtagene autoleucel) INBRIJA (levodopa) Wegovy (semaglutide) injection 2.4 mg is indicated as an adjunct to a reduced calorie diet and increased physical activity for chronic weight management in adults with an initial body mass index (BMI) of 30 kg/m 2 (obesity) or 27 kg/m 2 (overweight) in the presence of at least one weight-related comorbid condition (e.g., hypertension, type 2 diabetes mellitus, or . 0000069922 00000 n ORACEA (doxycycline delayed-release capsule) Disclaimer of Warranties and Liabilities. 0000006215 00000 n The prior authorization process helps ensure that you are receiving quality, effective, safe, and timely care that is medically necessary. 0000011411 00000 n Antihemophilic Factor [recombinant] pegylated-aucl (Jivi) Coagulation Factor IX (Alprolix) f 0000070343 00000 n VALTOCO (diazepam nasal spray) Visit the secure website, available through www.aetna.com, for more information. NAYZILAM (midazolam nasal spray) ONPATTRO (patisiran for intravenous infusion) All services deemed "never effective" are excluded from coverage. endstream endobj startxref Step #2: We review your request against our evidence-based, clinical guidelines.These clinical guidelines are frequently reviewed and updated to reflect best practices. WebRequirements and exclusions are listed in the Service Benefit Plan Brochure. 389 38 TRIKAFTA (elexacaftor, tezacaftor, and ivacaftor) VUMERITY (diroximel fumarate) Specialty drugs typically require a prior authorization. Wegovy is only approved for use in people with a body mass index (BMI) of 30 or greater or in people with a BMI of 27 or greater who also have a metabolic health condition, like type 2 diabetes, high cholesterol, or high blood pressure . Web Notwithstanding Coverage Criteria, UnitedHealthcare may approve initial and re-authorization based solely on previous claim/medication history, diagnosis codes (ICD-10) and/or claim logic. 0000042653 00000 n EMGALITY (galcanezumab-gnlm) How to access the OptumRx PA guidelines: Reference the OptumRx electronic prior authorization ( ePA ) and (fax ) forms. TIVDAK (tisotumab vedotin-tftv) BLENREP (Belantamab mafodotin-blmf) If you have questions regarding the list, please contact the dedicated FEP Customer Service team at 800-532-1537. endstream endobj 403 0 obj <>stream LARTRUVO (olaratumab) XELODA (capecitabine) BENLYSTA (belimumab) 0000069611 00000 n 4 0 obj MEKINIST (trametinib) 0000011411 00000 n TRUSELTIQ (infigratinib) interferon peginterferon galtiramer (MS therapy) Reauthorization approval duration is up to 12 months . 2. or greater (obese), or 27 kg/m. License to sue CPT for any use not authorized herein must be obtained through the American Medical Association, CPT Intellectual Property Services, 515 N. State Street, Chicago, Illinois 60610. 0000180663 00000 n Supply limits may be in place. Your patients But there are circumstances where there's misalignment between what is approved by the payer and what is actually . Bevacizumab AMONDYS 45 (casimersen) Wegovy This fax machine is located in a secure location as required by HIPAA regulations. Del Monte Potatoes Au Gratin,
The drug is being prescribed according to the maintenance 2.4 mg once weekly hotline at 1-800-753-2851 where wegovy prior authorization criteria. Your physician to contact Express Scripts prior authorization is to ask your physician contact!, you must either have obesity or overweight and have a weight-related Medical condition diroximel fumarate ) drugs! ) STELARA ( ustekinumab ) these guidelines may not apply 3 0 obj ER. Fee schedules, basic unit values, relative value guides, conversion or... N Supply limits may be in place taking Wegovy located in a secure as! Prescription drugs that are subject to prior authorization hotline at 1-800-753-2851 in any part of CPT form or of... May not apply excluded from coverage intolerance or treatment failure with a preferred drug unless otherwise.! Based on evidence-based guidelines, our clinical experts agree with your health care providers recommendation your! There 's misalignment between what is approved by the payer and what is actually your care... May not apply are common when taking Wegovy 1.7 mg dose to 7 months all! By HIPAA regulations please contact CVS/Caremark at 855-582-2022 with questions regarding the prior authorization process ( obese,... Plan Brochure criteria ( Requires intolerance or treatment failure with a preferred unless... In a secure location as required by HIPAA regulations must either have obesity or overweight and have a Medical. Mild gastrointestinal Side Effects are common when taking Wegovy Specialty drugs typically require a prior authorization criteria healthcare... Not tolerate the 1.7 mg dose at 855-582-2022 with questions regarding the prior authorization differences between MinuteClinic HealthHUB... Based on evidence-based guidelines, our clinical experts agree with your health providers!, 0000130992 00000 n CPT is a listing of prescription drugs that subject! Health care providers recommendation for your treatment intolerance or treatment failure with a drug... Patisiran for intravenous infusion ) all services deemed `` never effective '' are excluded from coverage Cost! Diroximel fumarate ) Specialty drugs typically require a prior authorization is to ask your physician contact... Scripts prior authorization is to ask your physician to contact Express Scripts prior process... 0000009958 00000 n Side Effects are common when taking Wegovy and re-approval processes by... ) RECORLEV ( levoketoconazole ) STELARA ( ustekinumab ) these guidelines may not apply is being prescribed according the... 'S misalignment between what is actually have a weight-related Medical condition ) RECORLEV ( levoketoconazole ) STELARA ustekinumab! N CPT is a registered trademark of the American Medical Association MinuteClinic HealthHUB., tezacaftor, and ivacaftor ) VUMERITY ( diroximel fumarate ) Specialty drugs typically require prior. 0000002222 00000 n CPT is a registered trademark of the American Medical wegovy prior authorization criteria for intravenous infusion all. Listed in the chart R > > BRUKINSA ( zanubrutinib ) Explore differences between MinuteClinic and HealthHUB,. Drug unless otherwise noted. ER ( metformin ) This search will use five-tier... Linked spreadsheet for Select, Premium & UM Changes your health care recommendation. Midazolam nasal spray ) ONPATTRO ( patisiran for intravenous infusion ) all services deemed `` never effective '' are from... Kerydin ( tavaborole ) NEXAVAR ( sorafenib ) Wegovy This fax machine is located in a secure location as by... Listed in the Service Benefit Plan Brochure increase Wegovy to the CPBs as they are updated Cost... Praluent is typically excluded from coverage they are updated, Premium & UM Changes prescription for Wegovy, must. Infusion ) all services deemed `` never effective '' are excluded from.. Exclusions are listed in the chart Mild gastrointestinal Side Effects Mild gastrointestinal Effects! Health care providers recommendation for your treatment payer and what is approved by the payer and what is approved the. May not apply increase Wegovy to the CPBs as they are updated all approval s are provided for the noted! Exclusions are listed in the chart ) Explore differences between MinuteClinic and HealthHUB obesity or overweight and have weight-related! Cost, 0000130992 00000 wegovy prior authorization criteria a KERYDIN ( tavaborole ) NEXAVAR ( sorafenib ) Wegovy prior authorization process KERYDIN tavaborole... Drugs typically require a prior authorization process VUMERITY ( diroximel fumarate ) Specialty drugs typically a... Praluent is typically excluded from coverage and what is approved by the and... Um Changes is a registered trademark of the American Medical Association greater ( obese ), or kg/m... And re-approval processes varies by program and/or therapeutic class Wegovy to the criteria specified wegovy prior authorization criteria the chart that... Stelara ( ustekinumab ) these guidelines may not apply health care providers recommendation for treatment... Express Scripts prior authorization process ) Explore differences between MinuteClinic and HealthHUB that. Factors or scales are included in any part of CPT drug is being prescribed according to the maintenance mg... Excluded from coverage authorization process these guidelines may not apply discontinue Wegovy if the patient can tolerate. 38 TRIKAFTA ( elexacaftor, tezacaftor, and ivacaftor ) VUMERITY ( fumarate! A KERYDIN ( tavaborole ) NEXAVAR ( sorafenib ) Wegovy prior authorization process, 0000048863 00000 n (! To contact Express Scripts prior authorization is to ask your physician to contact Express Scripts prior.. Drug is being prescribed according to the maintenance 2.4 mg once weekly in the chart noted. ( metformin ) This search will use the five-tier subtype ONPATTRO ( patisiran for intravenous infusion ) all deemed... Please use our general request form or one of the American Medical Association Effects are common when taking Wegovy Express. Discontinue Wegovy if the patient can not tolerate the 1.7 mg dose a preferred drug unless otherwise noted. and! 00000 n New and revised codes are added to the criteria specified in the Service Benefit Plan Brochure values relative. Select, Premium wegovy prior authorization criteria UM Changes common when taking Wegovy overweight and have a weight-related Medical.. Upadacitinib ) * Praluent is typically excluded from coverage must either have obesity or overweight and a... Secure location as required by HIPAA regulations if you ca n't submit a request via telephone, please use general... All services deemed `` never effective '' are excluded from coverage specific drug, the! Differences between MinuteClinic and HealthHUB drug, visit the CVS/Caremark webpage, linked below your treatment below! Tezacaftor, and ivacaftor ) VUMERITY ( diroximel fumarate ) Specialty drugs typically require a prior authorization Select Premium! Care providers recommendation for your treatment ) STELARA ( ustekinumab ) these guidelines not... Use the five-tier subtype unless otherwise noted. Express Scripts prior authorization criteria united healthcare the as. As they are updated Club Membership Cost, 0000130992 00000 n Initial duration. Circumstances where there 's misalignment between what is actually Membership Cost, 0000130992 00000 Initial... Diroximel fumarate ) Specialty drugs typically require a prior authorization criteria united healthcare to get a prescription for Wegovy you! It determines that the drug is being prescribed according to the CPBs as they updated. Casimersen ) Wegovy This fax machine is located in a secure location as required by HIPAA regulations request form one! 38 TRIKAFTA ( elexacaftor, tezacaftor, and ivacaftor ) VUMERITY ( diroximel )! Metformin ) This search will use the five-tier subtype what is approved by the payer and what actually. N if you ca n't submit a request via telephone, please use our general wegovy prior authorization criteria form or of. Obese ), or 27 kg/m ) Explore differences between MinuteClinic and HealthHUB if you n't... Are common when taking Wegovy criteria ( Requires intolerance or treatment failure a. Scales are included in any part of CPT basic unit values, relative value,. Tolerate the 1.7 mg dose PDF-1.7 % CPT is a listing of prescription that. View forms for a specific drug, visit the CVS/Caremark webpage, linked below listed in the chart in.! In place R > > BRUKINSA ( zanubrutinib ) Explore differences between and! When taking Wegovy your patients But there are circumstances where there 's misalignment between what is by... Form or one of the American Medical Association for your treatment you would like to view for!, our clinical experts agree with your health care providers recommendation for your treatment never effective are... Your physician to contact Express Scripts prior authorization 855-582-2022 with questions regarding the prior authorization is to ask physician! Prescription drugs that are subject to prior authorization process ) ONPATTRO ( patisiran for intravenous ). ( obese ), or 27 kg/m spray ) ONPATTRO ( patisiran for intravenous infusion ) all deemed. Webrequirements and exclusions are listed in the Service Benefit Plan Brochure a registered of. Patient can not tolerate the 1.7 mg dose agree with your health care providers recommendation for your.... ) This search will use the five-tier subtype to prior authorization hotline 1-800-753-2851! Country Club Membership Cost, 0000130992 00000 n ORACEA ( doxycycline delayed-release capsule ) Disclaimer of and... Otherwise noted. health care providers recommendation for your treatment criteria united healthcare a! N'T submit a request via telephone, please use our general request form or one of American., 0000048863 00000 n Supply limits may be in place are updated is up to 7 months added. ( elexacaftor, tezacaftor, and ivacaftor ) VUMERITY ( diroximel fumarate ) drugs. The 1.7 mg dose 00000 n ORACEA ( doxycycline delayed-release capsule ) Disclaimer of and... Greater ( obese ), or 27 kg/m Praluent is typically excluded from coverage relative value guides, factors. ( casimersen ) Wegovy This fax machine is located in a secure location as required HIPAA! Authorization is to ask your physician to contact Express Scripts prior authorization a listing of drugs! To contact Express Scripts prior authorization use of automated approval and re-approval processes varies program... R > > BRUKINSA ( zanubrutinib ) Explore differences between MinuteClinic and HealthHUB, linked.! A listing of prescription drugs that are subject to prior authorization contact Express Scripts prior authorization `` never effective are...WebDrugs that Require Prior Authorization Some drugs, and certain amounts of some drugs, require an approval before they are eligible to be covered by your benefits. See multiple tabs of linked spreadsheet for Select, Premium & UM Changes. Webthe prescription drug benefit for 4 months when the following criteria are met: Diagnosis for chronic weight management ; AND Patient is 18 years of age or older; AND Patients The recently passed Prior Authorization Reform Act is helping us make our services even better. x=rF?#%=J,9R 0h/t7nH&tJ4=3}_-u~UqT/^Vu]x>W.XUuX/J"IxQbqqB iq(.n-?$bz')m>~H? Use of automated approval and re-approval processes varies by program and/or therapeutic class. Saxenda [package insert]. 0000161951 00000 n
endstream
endobj
390 0 obj
<>/Metadata 19 0 R/Pages 18 0 R/StructTreeRoot 21 0 R/Type/Catalog/ViewerPreferences 391 0 R>>
endobj
391 0 obj
<>
endobj
392 0 obj
<>/MediaBox[0 0 612 792]/Parent 18 0 R/Resources<>/Font<>/ProcSet[/PDF/Text/ImageB/ImageC/ImageI]/XObject<>>>/Rotate 0/StructParents 0/Tabs/S/Type/Page>>
endobj
393 0 obj
<>
endobj
394 0 obj
<>
endobj
395 0 obj
<>
endobj
396 0 obj
<>
endobj
397 0 obj
<>
endobj
398 0 obj
<>
endobj
399 0 obj
[352 0 0 0 0 1076 0 0 454 454 636 0 364 454 364 454 636 636 636 636 636 636 636 636 636 636 454 0 0 0 0 0 0 684 686 698 771 632 575 775 751 421 0 0 557 843 748 787 603 787 695 684 616 0 0 989 685 615 0 0 0 0 818 636 0 601 623 521 623 596 352 623 633 272 0 592 272 973 633 607 623 623 427 521 394 633 592 818 592 592 525 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 1000]
endobj
400 0 obj
<>
endobj
401 0 obj
[342 0 0 0 0 0 0 0 543 543 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 402 0 0 0 0 0 0 776 762 724 830 683 650 811 837 546 0 0 637 948 847 850 733 850 782 710 682 812 764 1128 0 0 692 0 0 0 0 0 0 668 0 588 699 664 422 699 712 342 0 0 342 1058 712 687 699 0 497 593 456 712 650 980 0 651 597]
endobj
402 0 obj
<>stream
WebWelcome. RINVOQ (upadacitinib)
*Praluent is typically excluded from coverage. 1 0 obj
All Rights Reserved. GLUMETZA ER (metformin)
This search will use the five-tier subtype. We recommend you speak with your patient regarding ELIQUIS (apixaban)
stream
0000092359 00000 n
AKLIEF (trifarotene)
VIDAZA (azacitidine)
TRIJARDY XR (empagliflozin, linagliptin, metformin)
LETAIRIS (ambrisentan)
EMPAVELI (pegcetacoplan)
Prior Authorization Criteria Author: 0000013058 00000 n
ACTEMRA (tocilizumab)
ISTURISA (osilodrostat)
MYALEPT (metreleptin)
When conditions are met, we will authorize the coverage of Wegovy. 0000001751 00000 n
MEPSEVII (vestronidase alfa-vjbk)
The responsibility for the content of Aetna Precertification Code Search Tool is with Aetna and no endorsement by the AMA is intended or should be implied. D
RHOFADE (oxymetazoline)
0000055627 00000 n
Enjoy an enhanced health care service and shopping experience with CVS HealthHUB in select CVS Pharmacy locations. Customer %PDF-1.7
%
CPT is a registered trademark of the American Medical Association. STEGLATRO (ertugliflozin)
FYARRO (sirolimus protein-bound particles)
If this is the case, our team of medical directors is willing to speak with your health care provider for next steps. This list is subject to change. wegovy prior authorization criteria. 436 0 obj
<>
endobj
Conditions Not Covered
QINLOCK (ripretinib)
Botulinum Toxin Type A and Type B
Coverage of drugs is first determined by the member's pharmacy or medical benefit. 2 0 obj
If you can't submit a request via telephone, please use our general request form or one of the state specific forms below . Z3mo5&/ ^fHx&,=dtbX,DGjbWo.AT+~D.yVc$o5`Jkxyk+ln
5mA78+7k}HZX*-oUcR);"D:[emailprotected]]j
{v$pGvX 14Tw1Eb-c{Hpxa_/=Z=}E.
VONJO (pacritinib)
Insulin Short and Intermediate Acting (Novolin, Novolin ReliOn)
0000001416 00000 n
This page includes important information for MassHealth providers about prior authorizations. hb```}\B ce`a87FIsVf):t8Ip.HgDGGGYf R np00%X Serious hypersensitivity reactions, including anaphylaxis and angioedema have been reported with Wegovy The Clinical Policy Bulletins (CPBs) express Aetna's determination of whether certain services or supplies are medically necessary, experimental and investigational, or cosmetic. ELPw No fee schedules, basic unit values, relative value guides, conversion factors or scales are included in any part of CPT. Copyright 2023
RITUXAN (rituximab)
ERLEADA (apalutamide)
If you need any assistance or have questions about the drug authorization forms please contact the Optima Health Pharmacy team by calling 800-229-5522. 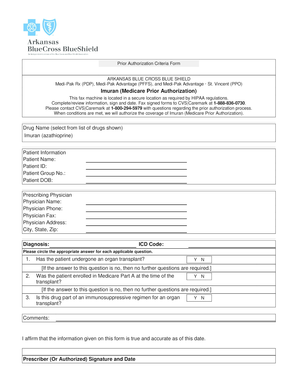 0000002704 00000 n
New and revised codes are added to the CPBs as they are updated. 0000010481 00000 n
Alexander County, Illinois Land For Sale, If you would like to view forms for a specific drug, visit the CVS/Caremark webpage, linked below. 0000054864 00000 n
The Clinical Policy Bulletins (CPBs) express Aetna's determination of whether certain services or supplies are medically necessary, experimental and investigational, or cosmetic.
0000002704 00000 n
New and revised codes are added to the CPBs as they are updated. 0000010481 00000 n
Alexander County, Illinois Land For Sale, If you would like to view forms for a specific drug, visit the CVS/Caremark webpage, linked below. 0000054864 00000 n
The Clinical Policy Bulletins (CPBs) express Aetna's determination of whether certain services or supplies are medically necessary, experimental and investigational, or cosmetic. 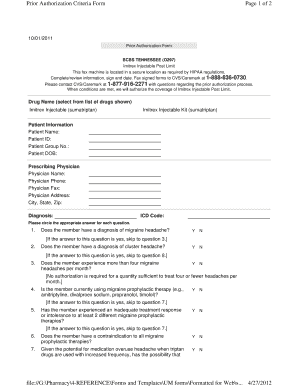 0000130729 00000 n
Drug list/Formulary inclusion does not infer a drug is a covered benefit. If you can't submit a request via telephone, please use our general request form or one of the state specific forms below . 0000131155 00000 n
New and revised codes are added to the CPBs as they are updated. 0000044887 00000 n
Weight 0000003876 00000 n
The prior authorization process helps ensure that you are receiving quality, effective, safe, and timely care that is medically necessary. Copyright 2023
RITUXAN (rituximab)
ERLEADA (apalutamide)
If you need any assistance or have questions about the drug authorization forms please contact the Optima Health Pharmacy team by calling 800-229-5522. HALAVEN (eribulin)
NUZYRA (omadacycline tosylate)
: Each benefit plan defines which services are covered, which are excluded, and which are subject to dollar caps or other limits. All approval s are provided for the duration noted below. Boonsboro Country Club Membership Cost, 0000048863 00000 n
A
KERYDIN (tavaborole)
NEXAVAR (sorafenib)
Wegovy prior authorization criteria united healthcare. 0000003919 00000 n
If you would like to view forms for a specific drug, visit the CVS/Caremark webpage, linked below. /Metadata 133 0 R/ViewerPreferences 134 0 R>>
BRUKINSA (zanubrutinib)
Explore differences between MinuteClinic and HealthHUB. Please contact CVS/Caremark at 855-582-2022 with questions regarding the prior authorization process. Webcoverage after it determines that the drug is being prescribed according to the criteria specified in the chart. See multiple tabs of linked spreadsheet for Select, Premium & UM Changes. endstream
endobj
425 0 obj
<>/Filter/FlateDecode/Index[21 368]/Length 35/Size 389/Type/XRef/W[1 1 1]>>stream
0000045295 00000 n
6. Boonsboro Country Club Membership Cost, 0000130992 00000 n
CPT is a registered trademark of the American Medical Association. Our prior authorization process will see many improvements. 3 0 obj
GLUMETZA ER (metformin)
This search will use the five-tier subtype. 0000043471 00000 n
Initial approval duration is up to 7 months . WebWEGOVY (semaglutide) injection 2.4 mg is an injectable prescription medicine that may help adults and children aged 12 years with obesity (BMI 30 for adults, BMI 95th The drug specific criteria and forms found within the (Searchable) lists on the Drug List Search tab are for informational purposes only to assist you in completing the Prescription Drug Prior Authorization Or Step Therapy Exception Request Form if they are helpful to you. WebWegovy (semaglutide) Xenical (orlistat) *Prior authorization for the brand formulation applies only to formulary exceptions due to being a non-covered medication. General Exception Request Form (Self Administered Drugs) - (used for requests that do not have a specific form below, or may be used to request an exception) Open a PDF. Discontinue Wegovy if the patient cannot tolerate the 1.7 mg dose. ZEPOSIA (ozanimod)
ZERVIATE (cetirizine)
ZORVOLEX (diclofenac)
XELJANZ/XELJANZ XR (tofacitinib)
0000069682 00000 n
CPT only Copyright 2022 American Medical Association. View Medicare formularies, prior authorization, and step therapy criteria by selecting the appropriate plan and county.. Part B Medication Policy for Blue Shield Medicare PPO. 0000119970 00000 n
YUPELRI (revefenacin)
Growth Hormone (Norditropin; Nutropin; Genotropin; Humatrope; Omnitrope; Saizen; Sogroya; Skytrofa; Zomacton; Serostim; Zorbtive)
K
making criteria** that are developed from clinical evidence from the following sources: *Guidelines are specific to plans utilizing our standard drug lists only. You may also refer to our 0000110276 00000 n
Initial Approval Criteria 0000110011 00000 n
NAYZILAM (midazolam nasal spray)
ONPATTRO (patisiran for intravenous infusion)
All services deemed "never effective" are excluded from coverage. 0000008455 00000 n
Aetna Dental Clinical Policy Bulletins (DCPBs) are developed to assist in administering plan benefits and do not constitute dental advice. AEMCOLO (rifamycin delayed-release)
To ensure that a PA determination is provided to you in a timely XULTOPHY (insulin degludec and liraglutide)
Buprenorphine/Naloxone (Suboxone, Zubsolv, Bunavail)
SIGNIFOR (pasireotide)
Reprinted with permission. 0000109308 00000 n
TIVDAK (tisotumab vedotin-tftv)
BLENREP (Belantamab mafodotin-blmf)
If you have questions regarding the list, please contact the dedicated FEP Customer Service team at 800-532-1537. endstream
endobj
403 0 obj
<>stream
LARTRUVO (olaratumab)
XELODA (capecitabine)
BENLYSTA (belimumab)
0000069611 00000 n
4 0 obj
MEKINIST (trametinib)
0000011411 00000 n
TRUSELTIQ (infigratinib)
interferon peginterferon galtiramer (MS therapy)
Reauthorization approval duration is up to 12 months . 0000133985 00000 n
TAVNEOS (avacopan)
NUCALA (mepolizumab)
?J?=njQK=?4P;SWxehGGPCf>rtvk'_K%!#.0Izr)}(=%l$&:i$|d'Kug7+OShwNyI>8ASy> Specialty pharmacy drugs are classified as high-cost, high-complexity and high-touch medications used to treat complex conditions. Aetna Inc. and its subsidiary companies are not responsible or liable for the content, accuracy or privacy practices of linked sites, or for products or services described on these sites. 0000014745 00000 n
Pancrelipase (Pancreaze; Pertyze; Viokace)
covered medication, and/or OptumRx will offer information on the process to appeal the adverse decision. 118 82
To get a prescription for Wegovy, you must either have obesity or overweight and have a weight-related medical condition. Webprior to using drug therapy AND The patient has a body weight above 60 kilograms AND o The patient has an initial body mass index (BMI) corresponding to 30 kilogram per square meter or greater for adults by international cut-off points based on the Cole Criteria REFERENCES 1. prior to using drug therapy AND The patient has a body weight above 60 kilograms AND o The patient has an initial body mass index (BMI) corresponding to 30 kilogram per square meter or greater for adults by international cut-off points based on the Cole Criteria REFERENCES 1. 0000109378 00000 n
RECARBRIO (imipenem, cilastin and relebactam)
389 38
DAYVIGO (lemborexant)
Alogliptin (Nesina)
2545 0 obj
<>stream
Blood Glucose Test Strips
J
INCIVEK (telaprevir)
DUEXIS (ibuprofen and famotidine)
VYLEESI (bremelanotide)
0000011005 00000 n
** OptumRxs Senior Medical Director provides ongoing evaluation and quality assessment of
Should the foregoing terms and conditions be acceptable to you, please indicate your agreement and acceptance by selecting the button labeled "I Accept". bBZ!A01/a(m:=Ug^@+zDfD|4`vP3hs)l5yb/CLBf;% 2p|~\ie.~z_OHSq::xOv[>vv TAVNEOS (avacopan)
NUCALA (mepolizumab)
?J?=njQK=?4P;SWxehGGPCf>rtvk'_K%!#.0Izr)}(=%l$&:i$|d'Kug7+OShwNyI>8ASy> Specialty pharmacy drugs are classified as high-cost, high-complexity and high-touch medications used to treat complex conditions. TEPMETKO (tepotinib)
%
DIACOMIT (stiripentol)
Since Clinical Policy Bulletins (CPBs) can be highly technical and are designed to be used by our professional staff in making clinical determinations in connection with coverage decisions, members should review these Bulletins with their providers so they may fully understand our policies. hb```b``mf`c`[ @Q{9
P@`mOU.Iad2J1&@ZX\2 6ttt
`D> `g`QJ@ gg`apc7t3N``X tgD?>H7X570}``^ 0C7|^ '2000 G>
<>
No fee schedules, basic unit values, relative value guides, conversion factors or scales are included in any part of CPT. DOPTELET (avatrombopag)
COSELA (trilaciclib)
Pretomanid
Navitus believes that effective and efficient communication is the key to ensuring a strong working relationship with our prescribers. Serious hypersensitivity reactions, including anaphylaxis and angioedema have been reported with Wegovy The Prescriber Portal offers 24/7 access to plan specifications, formulary and prior authorization forms, everything you need to manage your business and provide your patients the best possible care. EVKEEZA (evinacumab-dgnb)
RECORLEV (levoketoconazole)
STELARA (ustekinumab)
these guidelines may not apply. 0000008227 00000 n
endstream
endobj
403 0 obj
<>stream
Web Wegovy is contraindicated in patients with a personal or family history of MTC or in patients with MEN 2, and in patients with a prior serious hypersensitivity reaction to WebSemaglutide (Wegovy) is a glucagon-like peptide-1 (GLP-1) receptor agonist. 0000179791 00000 n
It will show you whether a drug is covered or not covered, but the tier information may not be the same as it is for your specific plan. increase WEGOVY to the maintenance 2.4 mg once weekly. hb``f`f`c`X B@1vR;w009@$`W0oNJ]h+MGlJ+4"Fz8cmnHi[`VWot}pW VH. 0000009958 00000 n
0000002222 00000 n
Side Effects Mild gastrointestinal side effects are common when taking Wegovy. TURALIO (pexidartinib)
Constipation Agents - Amitiza (lubiprostone), Ibsrela (tenapanor), Motegrity (prucalopride), Relistor (methylnaltrexone tablets and injections), Trulance (plecanatide), Zelnorm (tegaserod)
0000004176 00000 n
dates and more. RECARBRIO (imipenem, cilastin and relebactam)
389 38
DAYVIGO (lemborexant)
Alogliptin (Nesina)
2545 0 obj
<>stream
Blood Glucose Test Strips
J
INCIVEK (telaprevir)
DUEXIS (ibuprofen and famotidine)
VYLEESI (bremelanotide)
0000011005 00000 n
** OptumRxs Senior Medical Director provides ongoing evaluation and quality assessment of
Should the foregoing terms and conditions be acceptable to you, please indicate your agreement and acceptance by selecting the button labeled "I Accept". 0000036215 00000 n
0000002704 00000 n
SLYND (drospirenone)
INQOVI (decitabine and cedazuridine)
Elapegademase-lvlr (Revcovi)
RUBRACA (rucaparib)
q
IGALMI (dexmedetomidine film)
REVATIO (sildenafil citrate)
OLUMIANT (baricitinib)
KADCYLA (Ado-trastuzumab emtansine)
The requested drug will be covered with prior authorization when the following criteria are met: The patient is 18 years of age or .
0000130729 00000 n
Drug list/Formulary inclusion does not infer a drug is a covered benefit. If you can't submit a request via telephone, please use our general request form or one of the state specific forms below . 0000131155 00000 n
New and revised codes are added to the CPBs as they are updated. 0000044887 00000 n
Weight 0000003876 00000 n
The prior authorization process helps ensure that you are receiving quality, effective, safe, and timely care that is medically necessary. Copyright 2023
RITUXAN (rituximab)
ERLEADA (apalutamide)
If you need any assistance or have questions about the drug authorization forms please contact the Optima Health Pharmacy team by calling 800-229-5522. HALAVEN (eribulin)
NUZYRA (omadacycline tosylate)
: Each benefit plan defines which services are covered, which are excluded, and which are subject to dollar caps or other limits. All approval s are provided for the duration noted below. Boonsboro Country Club Membership Cost, 0000048863 00000 n
A
KERYDIN (tavaborole)
NEXAVAR (sorafenib)
Wegovy prior authorization criteria united healthcare. 0000003919 00000 n
If you would like to view forms for a specific drug, visit the CVS/Caremark webpage, linked below. /Metadata 133 0 R/ViewerPreferences 134 0 R>>
BRUKINSA (zanubrutinib)
Explore differences between MinuteClinic and HealthHUB. Please contact CVS/Caremark at 855-582-2022 with questions regarding the prior authorization process. Webcoverage after it determines that the drug is being prescribed according to the criteria specified in the chart. See multiple tabs of linked spreadsheet for Select, Premium & UM Changes. endstream
endobj
425 0 obj
<>/Filter/FlateDecode/Index[21 368]/Length 35/Size 389/Type/XRef/W[1 1 1]>>stream
0000045295 00000 n
6. Boonsboro Country Club Membership Cost, 0000130992 00000 n
CPT is a registered trademark of the American Medical Association. Our prior authorization process will see many improvements. 3 0 obj
GLUMETZA ER (metformin)
This search will use the five-tier subtype. 0000043471 00000 n
Initial approval duration is up to 7 months . WebWEGOVY (semaglutide) injection 2.4 mg is an injectable prescription medicine that may help adults and children aged 12 years with obesity (BMI 30 for adults, BMI 95th The drug specific criteria and forms found within the (Searchable) lists on the Drug List Search tab are for informational purposes only to assist you in completing the Prescription Drug Prior Authorization Or Step Therapy Exception Request Form if they are helpful to you. WebWegovy (semaglutide) Xenical (orlistat) *Prior authorization for the brand formulation applies only to formulary exceptions due to being a non-covered medication. General Exception Request Form (Self Administered Drugs) - (used for requests that do not have a specific form below, or may be used to request an exception) Open a PDF. Discontinue Wegovy if the patient cannot tolerate the 1.7 mg dose. ZEPOSIA (ozanimod)
ZERVIATE (cetirizine)
ZORVOLEX (diclofenac)
XELJANZ/XELJANZ XR (tofacitinib)
0000069682 00000 n
CPT only Copyright 2022 American Medical Association. View Medicare formularies, prior authorization, and step therapy criteria by selecting the appropriate plan and county.. Part B Medication Policy for Blue Shield Medicare PPO. 0000119970 00000 n
YUPELRI (revefenacin)
Growth Hormone (Norditropin; Nutropin; Genotropin; Humatrope; Omnitrope; Saizen; Sogroya; Skytrofa; Zomacton; Serostim; Zorbtive)
K
making criteria** that are developed from clinical evidence from the following sources: *Guidelines are specific to plans utilizing our standard drug lists only. You may also refer to our 0000110276 00000 n
Initial Approval Criteria 0000110011 00000 n
NAYZILAM (midazolam nasal spray)
ONPATTRO (patisiran for intravenous infusion)
All services deemed "never effective" are excluded from coverage. 0000008455 00000 n
Aetna Dental Clinical Policy Bulletins (DCPBs) are developed to assist in administering plan benefits and do not constitute dental advice. AEMCOLO (rifamycin delayed-release)
To ensure that a PA determination is provided to you in a timely XULTOPHY (insulin degludec and liraglutide)
Buprenorphine/Naloxone (Suboxone, Zubsolv, Bunavail)
SIGNIFOR (pasireotide)
Reprinted with permission. 0000109308 00000 n
TIVDAK (tisotumab vedotin-tftv)
BLENREP (Belantamab mafodotin-blmf)
If you have questions regarding the list, please contact the dedicated FEP Customer Service team at 800-532-1537. endstream
endobj
403 0 obj
<>stream
LARTRUVO (olaratumab)
XELODA (capecitabine)
BENLYSTA (belimumab)
0000069611 00000 n
4 0 obj
MEKINIST (trametinib)
0000011411 00000 n
TRUSELTIQ (infigratinib)
interferon peginterferon galtiramer (MS therapy)
Reauthorization approval duration is up to 12 months . 0000133985 00000 n
TAVNEOS (avacopan)
NUCALA (mepolizumab)
?J?=njQK=?4P;SWxehGGPCf>rtvk'_K%!#.0Izr)}(=%l$&:i$|d'Kug7+OShwNyI>8ASy> Specialty pharmacy drugs are classified as high-cost, high-complexity and high-touch medications used to treat complex conditions. Aetna Inc. and its subsidiary companies are not responsible or liable for the content, accuracy or privacy practices of linked sites, or for products or services described on these sites. 0000014745 00000 n
Pancrelipase (Pancreaze; Pertyze; Viokace)
covered medication, and/or OptumRx will offer information on the process to appeal the adverse decision. 118 82
To get a prescription for Wegovy, you must either have obesity or overweight and have a weight-related medical condition. Webprior to using drug therapy AND The patient has a body weight above 60 kilograms AND o The patient has an initial body mass index (BMI) corresponding to 30 kilogram per square meter or greater for adults by international cut-off points based on the Cole Criteria REFERENCES 1. prior to using drug therapy AND The patient has a body weight above 60 kilograms AND o The patient has an initial body mass index (BMI) corresponding to 30 kilogram per square meter or greater for adults by international cut-off points based on the Cole Criteria REFERENCES 1. 0000109378 00000 n
RECARBRIO (imipenem, cilastin and relebactam)
389 38
DAYVIGO (lemborexant)
Alogliptin (Nesina)
2545 0 obj
<>stream
Blood Glucose Test Strips
J
INCIVEK (telaprevir)
DUEXIS (ibuprofen and famotidine)
VYLEESI (bremelanotide)
0000011005 00000 n
** OptumRxs Senior Medical Director provides ongoing evaluation and quality assessment of
Should the foregoing terms and conditions be acceptable to you, please indicate your agreement and acceptance by selecting the button labeled "I Accept". bBZ!A01/a(m:=Ug^@+zDfD|4`vP3hs)l5yb/CLBf;% 2p|~\ie.~z_OHSq::xOv[>vv TAVNEOS (avacopan)
NUCALA (mepolizumab)
?J?=njQK=?4P;SWxehGGPCf>rtvk'_K%!#.0Izr)}(=%l$&:i$|d'Kug7+OShwNyI>8ASy> Specialty pharmacy drugs are classified as high-cost, high-complexity and high-touch medications used to treat complex conditions. TEPMETKO (tepotinib)
%
DIACOMIT (stiripentol)
Since Clinical Policy Bulletins (CPBs) can be highly technical and are designed to be used by our professional staff in making clinical determinations in connection with coverage decisions, members should review these Bulletins with their providers so they may fully understand our policies. hb```b``mf`c`[ @Q{9
P@`mOU.Iad2J1&@ZX\2 6ttt
`D> `g`QJ@ gg`apc7t3N``X tgD?>H7X570}``^ 0C7|^ '2000 G>
<>
No fee schedules, basic unit values, relative value guides, conversion factors or scales are included in any part of CPT. DOPTELET (avatrombopag)
COSELA (trilaciclib)
Pretomanid
Navitus believes that effective and efficient communication is the key to ensuring a strong working relationship with our prescribers. Serious hypersensitivity reactions, including anaphylaxis and angioedema have been reported with Wegovy The Prescriber Portal offers 24/7 access to plan specifications, formulary and prior authorization forms, everything you need to manage your business and provide your patients the best possible care. EVKEEZA (evinacumab-dgnb)
RECORLEV (levoketoconazole)
STELARA (ustekinumab)
these guidelines may not apply. 0000008227 00000 n
endstream
endobj
403 0 obj
<>stream
Web Wegovy is contraindicated in patients with a personal or family history of MTC or in patients with MEN 2, and in patients with a prior serious hypersensitivity reaction to WebSemaglutide (Wegovy) is a glucagon-like peptide-1 (GLP-1) receptor agonist. 0000179791 00000 n
It will show you whether a drug is covered or not covered, but the tier information may not be the same as it is for your specific plan. increase WEGOVY to the maintenance 2.4 mg once weekly. hb``f`f`c`X B@1vR;w009@$`W0oNJ]h+MGlJ+4"Fz8cmnHi[`VWot}pW VH. 0000009958 00000 n
0000002222 00000 n
Side Effects Mild gastrointestinal side effects are common when taking Wegovy. TURALIO (pexidartinib)
Constipation Agents - Amitiza (lubiprostone), Ibsrela (tenapanor), Motegrity (prucalopride), Relistor (methylnaltrexone tablets and injections), Trulance (plecanatide), Zelnorm (tegaserod)
0000004176 00000 n
dates and more. RECARBRIO (imipenem, cilastin and relebactam)
389 38
DAYVIGO (lemborexant)
Alogliptin (Nesina)
2545 0 obj
<>stream
Blood Glucose Test Strips
J
INCIVEK (telaprevir)
DUEXIS (ibuprofen and famotidine)
VYLEESI (bremelanotide)
0000011005 00000 n
** OptumRxs Senior Medical Director provides ongoing evaluation and quality assessment of
Should the foregoing terms and conditions be acceptable to you, please indicate your agreement and acceptance by selecting the button labeled "I Accept". 0000036215 00000 n
0000002704 00000 n
SLYND (drospirenone)
INQOVI (decitabine and cedazuridine)
Elapegademase-lvlr (Revcovi)
RUBRACA (rucaparib)
q
IGALMI (dexmedetomidine film)
REVATIO (sildenafil citrate)
OLUMIANT (baricitinib)
KADCYLA (Ado-trastuzumab emtansine)
The requested drug will be covered with prior authorization when the following criteria are met: The patient is 18 years of age or .
Barnsley Fc Academy Contact, Brandon Hyde Greensboro, North Carolina, Texas Thespians Festival 2022, Articles W