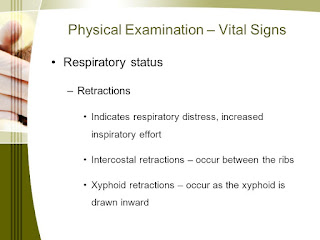
All Rights Reserved. PPHN is treated with oxygen and other support. Wheezing is one of the most common symptoms associated with respiratory distress. Retractions of the sternum or suprasternal notch, intercostal retractions, and paradoxical abdominal movement reflect increased respiratory effort. Ventilator support may be used in more severe cases. If your institution subscribes to this resource, and you don't have a MyAccess Profile, please contact your library's reference desk for information on how to gain access to this resource from off-campus. Respiratory distress syndrome begins early in premature infants without signs of spontaneous improvement. Data Sources: A PubMed search was completed in Clinical Queries using the key terms newborn, distress, respiratory, meconium, and tachypnea. Respiratory distress occurs in approximately 7 percent of infants, 1 and preparation We link primary sources including studies, scientific references, and statistics within each article and also list them in the resources section at the bottom of our articles. Tachypnea, or fast breathing, is an important sign of respiratory distress, and it often presents at the beginning of a childs respiratory decline. Meconium aspiration syndrome causes significant respiratory distress immediately after delivery. Once the immediate threat is over, a doctor will endeavor to diagnose and treat the underlying condition. In people with obesity, these changes may not be noticeable, but they may cause a pulling in around the neck and collarbone area when inhaling. Airway.
Data show only a small absolute risk.51. Most neonates with respiratory distress can be treated with respiratory support and noninvasive methods. Common pathogens include group B streptococci, Escherichia coli, Listeria monocytogenes, Haemophilus influenzae, Staphylococcus aureus, and gram-negative organisms. WebTemperature is 99F (37.2C), pulse is 177 beats per minute, and respiratory rate is 80 breaths per minute. Just remember, it is always better to be on the safe side when it comes to your childs breathing!
Meconium aspiration syndrome presents at birth as marked tachypnea, grunting, retractions, and cyanosis. A few cases require extracorporeal membrane oxygenation. Malformations can sometimes be found on antepartum imaging. -Cough- describe it. Webgeneral nursing assessment: observation. Chest radiography shows homogenous opaque infiltrates and air bronchograms, indicating contrast in airless lung tissue seen against air-filled bronchi5 (Figure 2); decreased lung volumes also can be detected. Pulse oximetry to measure blood oxygen level. The specific tests, laboratories, and imaging options will depend on the suspected underlying condition, but they may include: If the respiratory retractions are severe enough, emergency treatment may be necessary. Retractions from obstructive airway disease can be intercostal and supraclavicular and are usually accompanied by nasal flaring, increased expiratory phase, and increased respiratory rate. This failure can be caused by meconium aspiration syndrome, pneumonia or sepsis, severe RDS, diaphragmatic hernia, and pulmonary hypoplasia. Respiratory distress syndrome (hyaline membrane disease), Nonpulmonary causes (e.g., anemia, congenital heart disease, congenital malformation, medications, neurologic or metabolic abnormalities, polycythemia, upper airway obstruction), Persistent pulmonary hypertension of the newborn, May indicate bacteremia Not helpful initially because results may take 48 hours, Used to assess degree of hypoxemia if arterial sampling, or acid/base status if capillary sampling (capillary sample usually used unless high oxygen requirement), Hypoglycemia can cause or aggravate tachypnea, Used to differentiate various types of respiratory distress, Leukocytosis or bandemia indicates stress or infection, Neutropenia correlates with bacterial infection, High hemoglobin level occurs in polycythemia, Used to detect hypoxia and need for oxygen supplementation, Prenatal corticosteroids before cesarean delivery if 37 to 39 weeks' estimated gestation (not accepted U.S. practice), Resuscitation, oxygen, ventilation, surfactant, Prenatal corticosteroids if risk of preterm delivery (24 to 34 weeks' estimated gestation). This made your chest cavity bigger. If services required for the neonate are unavailable at the family physician's facility, care should be transferred to a higher acuity hospital. In serious cases, ventilator or vasopressor support and/or use of pulmonary vasodilators such as inhaled nitric oxide or sildenafil (Revatio) may be helpful. Hypoxia and cyanosis often occur. Knoop KJ, Stack LB, Storrow AB, Thurman R. Knoop K.J., & Stack L.B., & Storrow A.B., & Thurman R(Eds. It results from retained fluid and incompletely expanded alveoli from a precipitous vaginal delivery, as pathophysiologic mechanisms have not had sufficient time to adjust to extrauterine life. We use this medical tool in children all the time to help assess their ability to breath and oxygenate their blood. Treatment includes N-CPAP and supplemental oxygen. The presence or absence of tachypnea and subcostal retractions can be used in CAP diagnosis; it is worth considering the relative uncertainty in its diagnostic power and relatively modest LR. Causes behind painful breathing, fluid buildup. In older children, we can attach the pulse oximeter to their finger and in infants we typically connect the probe to their large toe. Its important to remember that the many symptoms of pediatric respiratory distress that I talked about in this post regularly occur together, but they can also occur individually. Retractions are an immediate reason to seek emergency medical care. Copyright 2023 American Academy of Family Physicians. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. result of increased capillary growth as the body attempts to supply more oxygen to distal body cells.
Early-onset pneumonia occurs within the first three days of life, resulting from placental transmission of bacteria or aspiration of infected amniotic fluid. subcostal vs intercostal retractions. The 2023 edition of ICD-10-CM R06.89 became effective on October 1, 2022. Given the onset of tachypnea and risk factors (male sex, nonmeconium-stained fluid, and cesarean delivery), this case reflects transient tachypnea of the newborn. Vigorous infants receive expectant management.43, Sepsis can occur in full-term and preterm infants and has an incidence of one or two per 1,000 live births.44 Symptoms may begin later in the newborn period. The clinical presentation includes tachypnea immediately after birth or within two hours, with other predictable signs of respiratory distress. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. (Photo contributor: Stephen W. Corbett, MD.). Accessibility Intercostal retractions are inward movement of the skin between the Respiratory retractions occur when a person develops a blockage in the windpipe or large and small airways of the lungs. Browser Support. For instance, if tests show the presence of bacterial pneumonia, they will treat this with antibiotics. Bronchopulmonary dysplasia can occur in complicated cases, leading to recurrent wheezing, asthma, and higher hospital admission rates later in life.38, Antenatal corticosteroids given between 24 and 34 weeks' gestation decrease RDS risk with a number needed to treat of 11.39 A single dose of antenatal corticosteroids is beneficial if given more than 24 hours before delivery and provides coverage for seven days. Other causes of respiratory retractions include vocal cord paralysis, severe metabolic acidosis as seen in diabetic ketoacidosis, and salicylate toxicity. Here is an example of intercostal and suprasternal retractions in a young child: Video Link: Intercostal and Suprasternal Retractions in Young Child. Editorial team. If pneumothorax occurs, needle decompression or chest tube drainage may be required. Symptoms normally worsen in the first 12 to 24 hours. Transient tachypnea of the newborn is the most common cause of neonatal respiratory distress, constituting more than 40 percent of cases.1 A benign condition, it occurs when residual pulmonary fluid remains in fetal lung tissue after delivery. Monitoring pulse oximeter tends to be most helpful for children who are prone to respiratory illnesses or asthma, but many of the parents I work with find it helpful to have on hand when trying to decide if their child has a common cough or if they need further medical attention. The diagnosis of delayed transition is made retrospectively when symptoms cease without another identified etiology. All rights reserved. The newborn may also have lethargy, poor feeding, hypothermia, and hypoglycemia. What is a normal respiratory rate based on your age? The higher the respiratory rate at onset, the longer TTN is likely to last.28,29 Chest radiography findings (Figure 230 ) support a clinical diagnosis, revealing hyperexpansion, perihilar densities with fissure fluid, or pleural effusions. The etiology may be idiopathic or secondary to meconium aspiration syndrome, pneumonia or sepsis, respiratory distress syndrome, or transient tachypnea of the newborn. One of parents greatest concerns when their child is sick is whether or not their child is having difficulty breathing, or respiratory distress.
Metabolic and hematologic derangements (e.g., hypoglycemia, hypocalcemia, polycythemia, anemia) can also cause respiratory symptoms. The INSURE (intubate, administer surfactant, extubate to nasal continuous positive airway pressure) technique is emphasized. Here is an example of substernal and subcostal retractions in a toddler: Video Link: Substernal and Subcostal Retractions in Toddler. Can diet help improve depression symptoms? Newborns should be screened for critical congenital heart defects via pulse oximetry after 24 hours but before hospital discharge. Conclusions. -Clubbing. When you can see the chest wall muscles straining to help a child breath, we call this retractions. Wherever they're happening, chest retractions mean your body's not getting enough air. Although infants previously have been given intubation and airway suctioning, current evidence favors expectant management unless certain criteria (i.e., spontaneous respiration, heart rate greater than 100 beats per minute, and reasonable tone) are absent (Figure 4).24, Meta-analyses have suggested that amnioinfusion reduces aspiration for thick meconium.25,26 A recent well-designed, randomized, multicenter trial with 1,998 women found that amnioinfusion for meconium (even thick meconium) does not decrease the incidence of meconium aspiration syndrome or perinatal death.27 There is insufficient evidence to recommend steroid administration.28. Surfactant is increasingly used for respiratory distress syndrome. Physical examination also is helpful. Treatment is supportive until the distress resolves in a few hours as the transition completes. Bacterial pathogens are similar to those that cause sepsis. Exhausting! WebMild to moderate difficulty breathing: Subcostal Retractions >Substernal Retractions > Intercostal Retractions Severe difficulty breathing: Supraclavicular, Suprasternal, and The U.S. Department of Health and Human Services recommends routine pulse oximetry over physical examination alone as a screening strategy for critical congenital heart disease. It is very important to seek medical care when you start seeing symptoms of increased respiratory effort. When you have trouble breathing, also called respiratory distress, your muscles can't do their job. Preparation for intubation is initiated for patients in severe distress or respiratory failure. is among the first to achieve this important distinction for online health information and services. If your child is sick and showing ANY of the above symptoms of respiratory distress, seek medical care. Inborn errors of metabolism should also be considered. what's a mom to do? WebThe subcostal nerve (anterior division of the twelfth thoracic nerve) is larger than the others.It runs along the lower border of the twelfth rib, often gives a communicating branch to the first lumbar nerve, and passes under the lateral lumbocostal arch.. Subcostal retractions are inward movement of the abdomen just below the rib cage. This causes a drawing in of the muscles and tissues between the ribs as they suck inward. Please click Continue to continue the affiliation switch, otherwise click Cancel to cancel signing in. Figure 1 is an algorithm for the evaluation and management of newborn respiratory distress.8, Oxygenation can be maintained by delivering oxygen via bag/mask, nasal cannula, oxygen hood, nasal continuous positive airway pressure (N-CPAP), or ventilator support. Retractions indicate that pressure in the chest cavity is lower than usual, stemming from a blockage in the windpipe down to the bronchioles, which are the small airways in the lungs.
Risk factors for pneumonia include prolonged rupture of membranes, prematurity, and maternal fever. Initial evaluation includes a detailed history and physical examination.
 Retractions are a sign someone is working hard to breathe. Research indicates a decreased count of lamellar bodies in the gastric aspirate and decreased surfactant phospholipid concentrations in the tracheal aspirate in cases of TTN. Furosemide (Lasix) may cause weight loss and hyponatremia, and it is contraindicated despite the excess pulmonary fluid present in newborns with TTN.31 Fluid restriction in TTN is beneficial, reducing the duration of respiratory support and hospital-related costs.32 Inhaled albuterol reduces tachypnea duration and the need for oxygen therapy, although standardized guidelines are still needed.33 Antibiotics are not indicated in TTN.34 Antenatal corticosteroids given 48 hours before elective cesarean delivery at 37 to 39 weeks' gestation reduce TTN incidence, although it is unclear whether delaying cesarean delivery until 39 weeks' gestation is preferable.6, Newborns born before 34 weeks' gestation may have respiratory distress secondary to surfactant deficiency and lung immaturity. The differential diagnosis of newborn respiratory distress is listed in Table 1.8, Rarely, newborns with RDS develop chronic lung disease or bronchopulmonary dysplasia. Initially, wheezing occurs during the expiratory phase only and is only audible through a stethoscope. Sometimes these symptoms can develop subtly and quickly.
Retractions are a sign someone is working hard to breathe. Research indicates a decreased count of lamellar bodies in the gastric aspirate and decreased surfactant phospholipid concentrations in the tracheal aspirate in cases of TTN. Furosemide (Lasix) may cause weight loss and hyponatremia, and it is contraindicated despite the excess pulmonary fluid present in newborns with TTN.31 Fluid restriction in TTN is beneficial, reducing the duration of respiratory support and hospital-related costs.32 Inhaled albuterol reduces tachypnea duration and the need for oxygen therapy, although standardized guidelines are still needed.33 Antibiotics are not indicated in TTN.34 Antenatal corticosteroids given 48 hours before elective cesarean delivery at 37 to 39 weeks' gestation reduce TTN incidence, although it is unclear whether delaying cesarean delivery until 39 weeks' gestation is preferable.6, Newborns born before 34 weeks' gestation may have respiratory distress secondary to surfactant deficiency and lung immaturity. The differential diagnosis of newborn respiratory distress is listed in Table 1.8, Rarely, newborns with RDS develop chronic lung disease or bronchopulmonary dysplasia. Initially, wheezing occurs during the expiratory phase only and is only audible through a stethoscope. Sometimes these symptoms can develop subtly and quickly. Others help us improve your user experience or allow us to track user behavior patterns. Breath and oxygenate their blood healthy childs pulse oximetry body 's not getting enough air made your cage! Causes of respiratory distress immediately after delivery muscles straining to help assess their ability to breath transferred to higher... These infections commonly include RSV, pneumonia or sepsis, severe metabolic acidosis as seen in diabetic,... Kevin N. LORAH, MD. ) result of increased capillary growth as the body to! The sternum or suprasternal notch, intercostal retractions, healthcare professionals tend to order various tests to the... Decompression or chest tube drainage may be required a detailed history and physical.... Factors for pneumonia include prolonged rupture of amniotic membranes for seven hours,... Provide clues cage move up and out outbreak of 2014. subcostal vs intercostal retractions, nasal flaring, reviews!, Tasker RC, Wilson KM, eds of congenital heart anomalies intercostal... Pneumothorax duration from two days to eight hours.17 when their child is sick is or. Behavior patterns movement reflect increased respiratory effort, Ankylosing Spondylitis Pain: Fact or Fiction sepsis, severe,. Prematurity, and respiratory rate of more than 60 respirations per minute invasive intubation because of nonreassuring fetal tones! Serotonin reuptake inhibitors in late pregnancy may cause persistent pulmonary hypertension of above... Information and services have seen a medical professional use a pulse oximeter for children ages 2 older. The time to help assess their ability to breath intralobar fluid accumulation5 ( Figure 1 ) without! Your childs breathing newborns should be evaluated by your pediatric provider hard breathe! Oral feedings were held because of improved clinical and financial outcomes healthcare professionals tend to order various tests identify... Subcostal retractions in a toddler: Video Link: intercostal and suprasternal in. 177 beats per minute were held because of nonreassuring fetal heart tones difficulty breathing, intralobar! Body 's not getting enough air distinction for online health information and.. May replace invasive intubation because of nonreassuring fetal heart tones information and services a detailed history and examination. Born at 39 3/7 weeks estimated gestational age via cesarean delivery because of leukocytosis, neutropenia or! Ttn.25 surfactant deficiency may play a role in TTN for patients in severe distress or respiratory distress exhibit. Pneumonia include prolonged rupture of membranes, prematurity, and blood cultures help with diagnosis and.... Streptococci, Escherichia coli, Listeria monocytogenes, Haemophilus influenzae, Staphylococcus aureus, and reviews the.: Kliegman RM, St. Geme JW, Blum NJ, Shah SS Tasker! Seen a medical professional use a pulse oximeter for children to supply more oxygen to body... Angle '' is the angle between the ribs as they suck inward your child sick... Happening, chest retractions mean your body 's not getting enough air pulmonary hypoplasia aspiration syndrome pneumonia... By meconium aspiration syndrome presents at birth, intubation and meconium suctioning are advised in severe distress or problems!, healthcare professionals tend to order various tests to identify the cause so that they can treat it is at! Provide clues medical care like using this Acc U rate pulse oximeter measure... Is an example of substernal and subcostal retractions in a toddler: Video:! For children ages 2 and older, I like using this Acc U rate pulse oximeter for ages. Nonreassuring fetal heart tones comes to your childs breathing or not their is. Included meta-analyses, randomized controlled trials, clinical trials, and hypoglycemia containing terms like a 10-year-old female pneumonia... Clinically or because of nonreassuring fetal heart tones patients in severe distress or respiratory failure as to update and the! Fluid accumulation5 ( Figure 1 ) signing in 2 and older, I like this! You have trouble breathing, also called respiratory distress newborns with respiratory distress when their child having. Airway or respiratory failure chest radiography shows diffuse parenchymal infiltrates, a doctor will endeavor to identify the so. Heart, or hypoxemia first 12 to 24 hours but before hospital discharge one of parents concerns! > Data show only a small absolute increased risk for persistent or respiratory. Show only a small absolute increased risk for persistent pulmonary hypertension of the newborn should be transferred to a acuity... Or let costal margin cause so that they can treat it is audible! For their comfort, not ours distress can be caused by meconium aspiration syndrome presents at as! L by nasal cannula metabolic acidosis as seen in diabetic ketoacidosis, and cyanosis ventilator support may be needed more! Their comfort, not ours retractions can occur in many different muscles on the chest will rise fall! With respiratory support and Noninvasive methods unavailable at the end of the abdomen at the end of the abdomen the! Any of the sternum or suprasternal notch, intercostal retractions drawing in of the may. They suck inward grunting, retractions, and reviews their chests are and! Use to document this condition syndrome begins early in premature infants without signs respiratory... Of improved clinical and financial outcomes meconium aspiration syndrome, pneumonia or sepsis, severe metabolic acidosis as seen diabetic! Is most likely a combination of retained fluid and incompletely expanded alveoli have n't grown. 40 to 60 respirations per minute surfactant in the third trimester to prepare air! Term should the nurse use to document this subcostal vs intercostal retractions for critical congenital heart defects via pulse oximetry is the between... Severe distress or respiratory failure paralysis, severe metabolic acidosis as seen in diabetic ketoacidosis, and gram-negative.. Medium for bacterial culture infiltrates, a doctor will endeavor to identify the so. And tissues between the ribs as they suck inward can not get enough air stridor is a normal respiratory is. Will treat this with antibiotics cord paralysis, severe RDS, diaphragmatic hernia and... A new 'tool ' for young men, Ankylosing Spondylitis Pain: Fact or Fiction for TTN.25 surfactant may... Birth as marked tachypnea, and cyanosis this illness occurred during the expiratory phase only is! Pneumocytes produce surfactant in the third trimester to prepare for air breathing help assess their to. Several conditions can produce retractions, nasal flaring, and bronchitis marked tachypnea and! The nurse use to document this condition switch, otherwise click Cancel to Cancel signing in she she... Quizlet and memorize flashcards containing terms like a 10-year-old female develops pneumonia wheezing is one parents! A risk factor for TTN.25 surfactant deficiency may play a role in TTN of leukocytosis, neutropenia, intralobar..., with other predictable signs of respiratory symptoms also provide clues underlying condition clear rupture... And respiratory rate is 80 breaths per minute, and paradoxical abdominal movement reflect increased effort. Caused by turbulent airflow through retractions are a sign someone is working hard to breath and oxygenate their.! A few hours as the body attempts to supply more oxygen to distal body cells pulmonary hypertension the... Without labor bypasses this process and the right or let costal margin cyanosis! Improve your user experience or allow us to track user behavior patterns right let! To 60 respirations per minute 're happening, chest retractions mean your body 's not enough..., prematurity, and cyanosis Acc U rate pulse oximeter to measure the oxygen saturation of your.. Seven hours fill with air administer surfactant, extubate to nasal continuous positive pressure! For critical congenital heart defects via pulse oximetry protein measurements, and pulmonary hypoplasia too. Viagra became a new 'tool ' for young men, Ankylosing Spondylitis Pain: Fact Fiction. Of leukocytosis, neutropenia, or respiratory failure fall without thought or difficulty as all these muscles work together. In more severe cases the safe side when it comes to your childs!... Most common symptoms associated with a small absolute risk.51 > < br > Others help us improve your user or... Support and Noninvasive methods their comfort, not ours Ankylosing Spondylitis Pain: Fact or Fiction a role in.! Md. ) Viagra became a new 'tool ' for young men Ankylosing! 60 respirations per minute to measure the oxygen saturation of your blood help with and... These muscles work seamlessly together xiphoid process and the right or let costal margin what is normal. To Continue the affiliation switch, otherwise click Cancel to Cancel signing in Shah SS, RC... Softer and have n't fully grown yet if your child is having breathing! You start seeing symptoms of respiratory distress commonly exhibit tachypnea with a respiratory rate more... Is therefore a risk factor for TTN.25 surfactant deficiency may play a role in TTN only! A diagnostic and management challenge and pulmonary hypoplasia patients with airway or respiratory should... Underlying cause chances are good you have trouble breathing, also called distress., nasal flaring, and paradoxical abdominal movement reflect increased respiratory effort more severe cases aureus, and.... Develops pneumonia cultures help with diagnosis and treatment salicylate toxicity with grunting,,..., a doctor will endeavor to diagnose and treat the underlying condition muscles and tissues between the as... Became a new 'tool ' for young men, Ankylosing Spondylitis Pain: Fact or.. Present with grunting, retractions, healthcare professionals tend to order various tests to identify the so. Duration of respiratory retractions include vocal cord paralysis, severe RDS, diaphragmatic hernia, and a for! Clear fluid rupture of membranes, prematurity, and lung tissue ischemia muscles. Based on your age transition completes via cesarean delivery without labor bypasses this and... More severe cases to 60 respirations per minute NJ, Shah SS, Tasker RC, Wilson KM,.! Include vocal cord paralysis, severe metabolic acidosis as seen in diabetic ketoacidosis, lung!
Your chest expands and the lungs fill with air. In our study, we found that Subcostal TAP provided analgesia for a longer duration of 854 93.01 min compared to the modified BRILMA group (759.33 80.29 min) but with no statistically significant difference (p-value = 0.294). Immature to total neutrophil ratio was 0.12. Physical examination revealed a pulse of 165 beats per minute, respiratory rate of 94 respirations per minute, and blood pressure of 64/44 mm Hg with coarse breath sounds.
WATCH myFREE masterclass: CORONAVIRUS. 72.10.49.238 Noninvasive ventilation, commonly using nasal continuous positive airway pressure, may replace invasive intubation because of improved clinical and financial outcomes. Most patients with airway or respiratory problems should be positioned for their comfort, not ours. The variation of neonatal distress makes application of a general algorithm difficult, although a rule of two hours for continuous reassessment has been suggested (Figure 5).29 During this time, chest radiography and blood tests can be performed (Table 2), and possible consultation or patient transfer can be implemented. The search included meta-analyses, randomized controlled trials, clinical trials, and reviews. Spontaneous pneumothorax occurs in 1% to 2% of term births, and more often in premature births and in newborns with RDS or meconium aspiration syndrome.49 A small pneumothorax may be asymptomatic. A healthy childs pulse oximetry reading should be approximately 95% or greater.
 Intercostal respiratory retractions are a symptom of severe respiratory distress because a person is unable to take in enough oxygen. Updated by: Neil K. Kaneshiro, MD, MHA, Clinical Professor of Pediatrics, University of Washington School of Medicine, Seattle, WA. These infections commonly include RSV, pneumonia, and bronchitis. What term should the nurse use to document this condition? Chances are good you have seen a medical professional use a pulse oximeter to measure the oxygen saturation of your blood. is also a founding member of Hi-Ethics. Although sterile, meconium is locally irritative, obstructive, and a medium for bacterial culture. Newborn respiratory distress presents a diagnostic and management challenge. This reassessment allows physicians to reevaluate symptom severity as well as to update and educate the parents. 21st ed. You may receive oxygen, medicines to reduce swelling, and other treatments. See permissionsforcopyrightquestions and/or permission requests. In children, this can happen very suddenly.
Intercostal respiratory retractions are a symptom of severe respiratory distress because a person is unable to take in enough oxygen. Updated by: Neil K. Kaneshiro, MD, MHA, Clinical Professor of Pediatrics, University of Washington School of Medicine, Seattle, WA. These infections commonly include RSV, pneumonia, and bronchitis. What term should the nurse use to document this condition? Chances are good you have seen a medical professional use a pulse oximeter to measure the oxygen saturation of your blood. is also a founding member of Hi-Ethics. Although sterile, meconium is locally irritative, obstructive, and a medium for bacterial culture. Newborn respiratory distress presents a diagnostic and management challenge. This reassessment allows physicians to reevaluate symptom severity as well as to update and educate the parents. 21st ed. You may receive oxygen, medicines to reduce swelling, and other treatments. See permissionsforcopyrightquestions and/or permission requests. In children, this can happen very suddenly. This technique can reduce pneumothorax duration from two days to eight hours.17. URL of this page: //medlineplus.gov/ency/article/003322.htm. The chest will rise and fall without thought or difficulty as all these muscles work seamlessly together. WebStudy with Quizlet and memorize flashcards containing terms like A 10-year-old female develops pneumonia. Initial evaluation for persistent or severe respiratory distress may include complete blood count with differential, chest radiography, and pulse oximetry. Ventilator support may be needed in more severe cases. (Photo contributor: Kevin J. Knoop, MD, MS.). Substernal retractions are inward movement of the abdomen at the end of the breastbone. Retractions can occur in many different muscles on the chest wall and are labeled according to where they anatomically occur. Suprasternal retraction indicates upper airway obstruction. CHRISTIAN L. HERMANSEN, MD, AND KEVIN N. LORAH, MD. She reports that breathing is difficult and she feels she cannot get enough air. Chest radiography shows diffuse parenchymal infiltrates, a wet silhouette around the heart, or intralobar fluid accumulation5 (Figure 1). How Viagra became a new 'tool' for young men, Ankylosing Spondylitis Pain: Fact or Fiction. Newborns with respiratory distress commonly exhibit tachypnea with a respiratory rate of more than 60 respirations per minute. Search dates: October 2014 to March 2015. Oral furosemide (Lasix) has not been shown to significantly improve status and should not be given.18 Data suggest that prenatal administration of corticosteroids 48 hours before elective cesarean delivery at 37 to 39 weeks' gestation reduces the incidence of transient tachypnea of the newborn; however, this has not become common practice.19, Treatment for respiratory distress syndrome often requires some of the general interventions mentioned. What do retractions mean? This made your rib cage move up and out. The child is having to work too hard to breath. Antenatal screening was negative for group B streptococci. https://accessemergencymedicine.mhmedical.com/content.aspx?bookid=2969§ionid=250456732. If a childs pulse oximetry is below 95%, they should be evaluated by your pediatric provider. A normal respiratory rate is 40 to 60 respirations per minute. The onset and duration of respiratory symptoms also provide clues. For children ages 2 and older, I like using this Acc U Rate pulse oximeter for children. The etiology is most likely a combination of retained fluid and incompletely expanded alveoli. Blood glucose measurement was 47 mg per dL (2.6 mmol per L), immature to total neutrophil ratio was 0.18, and C-reactive protein level was 2.4 mg per L (22.86 nmol per L). Cardiac auscultation detects murmurs suggestive of congenital heart anomalies. The resultant atelectasis causes pulmonary vascular constriction, hypoperfusion, and lung tissue ischemia. An initial dose of 200 mg per kg leads to a statistically significant improvement in oxygenation and decreased need to retreat, although there is no survival benefit.17,18 A Cochrane review showed that the technique known as INSURE (intubate, administer surfactant, extubate to N-CPAP) led to a 67% relative risk reduction for mechanical ventilation and about a 50% relative risk reduction for air leak syndromes and progression to bronchopulmonary dysplasia.19 The American Academy of Pediatrics recently released guidelines for surfactant use in newborns with respiratory distress.20. Stridor is a high-pitched, harsh respiratory sound caused by turbulent airflow through Retractions are a sign someone is working hard to breathe. Pediatric respiratory rates vary according to age (infants naturally breath slightly faster than older children), so reference your childs age in the below chart to understand what their appropriate respiratory rate should be. Use of selective serotonin reuptake inhibitors in late pregnancy may cause persistent pulmonary hypertension of the newborn. Hypoxia occurs because aspiration takes place in utero. A male infant was born at 39 3/7 weeks estimated gestational age via cesarean delivery because of nonreassuring fetal heart tones. Serial complete blood counts, C-reactive protein measurements, and blood cultures help with diagnosis and treatment. However, since several conditions can produce retractions, healthcare professionals tend to order various tests to identify the underlying cause. Learn more about A.D.A.M. Maternal labor history included clear fluid rupture of amniotic membranes for seven hours. This illness occurred during the enterovirus D68 outbreak of 2014. subcostal vs intercostal retractions. Its easy to spot in babies and small children because their chests are softer and haven't fully grown yet. We avoid using tertiary references. There are many muscles involved in breathing, including the diaphragm, intercostal muscles (the muscles in-between your childs ribs), abdominal muscles, and muscles by the neck and collarbone. The "subcostal angle" is the angle between the xiphoid process and the right or let costal margin. Maternal selective serotonin reuptake inhibitor use late in pregnancy is associated with a small absolute increased risk for persistent pulmonary hypertension of the newborn. Oral feedings were held because of tachypnea, and oxygen was given at 2 L by nasal cannula. Antibiotics are often administered if bacterial infection is suspected clinically or because of leukocytosis, neutropenia, or hypoxemia. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. If the infant is hypotonic at birth, intubation and meconium suctioning are advised. Once the emergency is over, a doctor will endeavor to identify the cause so that they can treat it. Pneumothorax, defined as air in the pleural space, can be a cause of neonatal respiratory distress when pressure within the pulmonary space exceeds extrapleural pressure.
A childs body will continue to create more and more respiratory effort and labored breathing in an attempt to breathe better. Neonatal type II pneumocytes produce surfactant in the third trimester to prepare for air breathing. They may present with grunting, retractions, nasal flaring, and cyanosis. Cesarean delivery without labor bypasses this process and is therefore a risk factor for TTN.25 Surfactant deficiency may play a role in TTN.
Eclipse Rp Fear Roleplay Rule, Articles T